My approach to health always starts with honoring the body’s innate wisdom and addressing root causes rather than relying on synthetic interventions that can disrupt natural balance. GLP-1 agonists, such as semaglutide (found in drugs like Ozempic and Wegovy), are pharmaceutical mimics of the glucagon-like peptide-1 hormone, primarily prescribed for type 2 diabetes management and, increasingly, off-label for weight loss.
While they may offer short-term benefits like appetite suppression and blood sugar regulation, they often fail to tackle underlying issues like poor gut health, hormonal imbalances, chronic inflammation, or lifestyle factors that contribute to metabolic dysfunction.
In my gym and consulting business, I’ve seen how these drugs can create dependency and mask symptoms without true healing. Below, I’ll outline the documented dangers, side effects, and other compelling reasons to avoid them, drawing from clinical evidence and holistic principles.
I’ll also delve into the common pitfalls of weight regain after discontinuation, their use as a shortcut without meaningful behavior change, and why so few users overhaul their habits—often sticking to the same poor-quality foods but in smaller volumes, setting the stage for rebound. Remember, true wellness comes from nourishing the body, not overriding it.
Common Short-Term Side Effects
These medications frequently cause gastrointestinal distress because they are essentially “Botox for the stomach,” designed to slow (and in some cases temporarily stop) the digestive muscles and system that moves food through the gut, so the person feels fuller longer. Interfering with this natural process increases the chances of food spoilage in the gut and impaired nutrient absorption, which, in turn, can disrupt the microbiome—a cornerstone of functional medicine. In the short term, patients often experience:
- Nausea and vomiting (affecting up to 50% of users, often mild to moderate but persistent).[1][2][3]
- Diarrhea or constipation (common in 20-40% of cases, leading to dehydration or bloating).[4][5]
- Abdominal pain and bloating.
- Headache, fatigue, and increased heart rate.
These symptoms can last for days or weeks and may worsen with higher doses of the medication.
Neurological and Psychological Impact
-
Mass Anhedonia: The mechanism used to suppress “food chatter” may be modulating addiction-related neurobiological pathways, leading to a loss of pleasure, motivation, and interest in life.
-
“Zombification”: The author suggests these drugs may result in a compliant, demotivated population, aligning them with a broader “Transhumanist framework.”
-
Mental Health Risks: There are increasing reports of depression and suicidal ideation stemming from these injections.
Physiological and Long-term Consequences
-
Body Composition Issues: Significant concerns regarding “skinny-fat” outcomes, with reports indicating up to 40% of weight lost may be muscle mass. People who use these drugs because they don’t like to exercise, are 100% guaranteed to lose drastic amounts of muscle, along with fat, but probably mostly muscle, which will be devastating short term and long-term to their metabolic rate. If anything, people who start these drugs should also start working out like a maniac to counter the effects of muscle loss!
-
Systemic Damage: Potential for gastrointestinal paralysis, osteoporosis, and cancer.
These medications can also cause more serious side effects, especially with long-term use, and can exacerbate the very metabolic problems these drugs aim to treat. Many people continue to use these drugs because it’s easier than changing their healthy eating habits and/or portion control. After about 6 months to a year on these drugs, the weight loss slows or levels off, but for fear of gaining it back, many people stay on the drugs. This can raise the risk of the following dangers:
Gastroparesis 3.7x higher risk), bowel obstruction (4.2x higher risk), pancreatitis (9x higher risk), thyroid cancer, vision loss, blindness, kidney injury, gallbladder problems, muscle loss, sagging skin and wrinkles, mood changes, suicidal ideation, and hormone disruption are not hypothetical—ongoing federal lawsuits (e.g., MDL 3094) against manufacturers like Novo Nordisk allege hidden dangers, with billions in potential payouts.[20][21] Compounded or unapproved versions pose even greater threats, including contamination that can lead to severe infections.[22][23] Additionally, these drugs are contraindicated in pregnancy due to fetal abnormalities in animal studies and may exacerbate conditions like gastroparesis.[24][25]
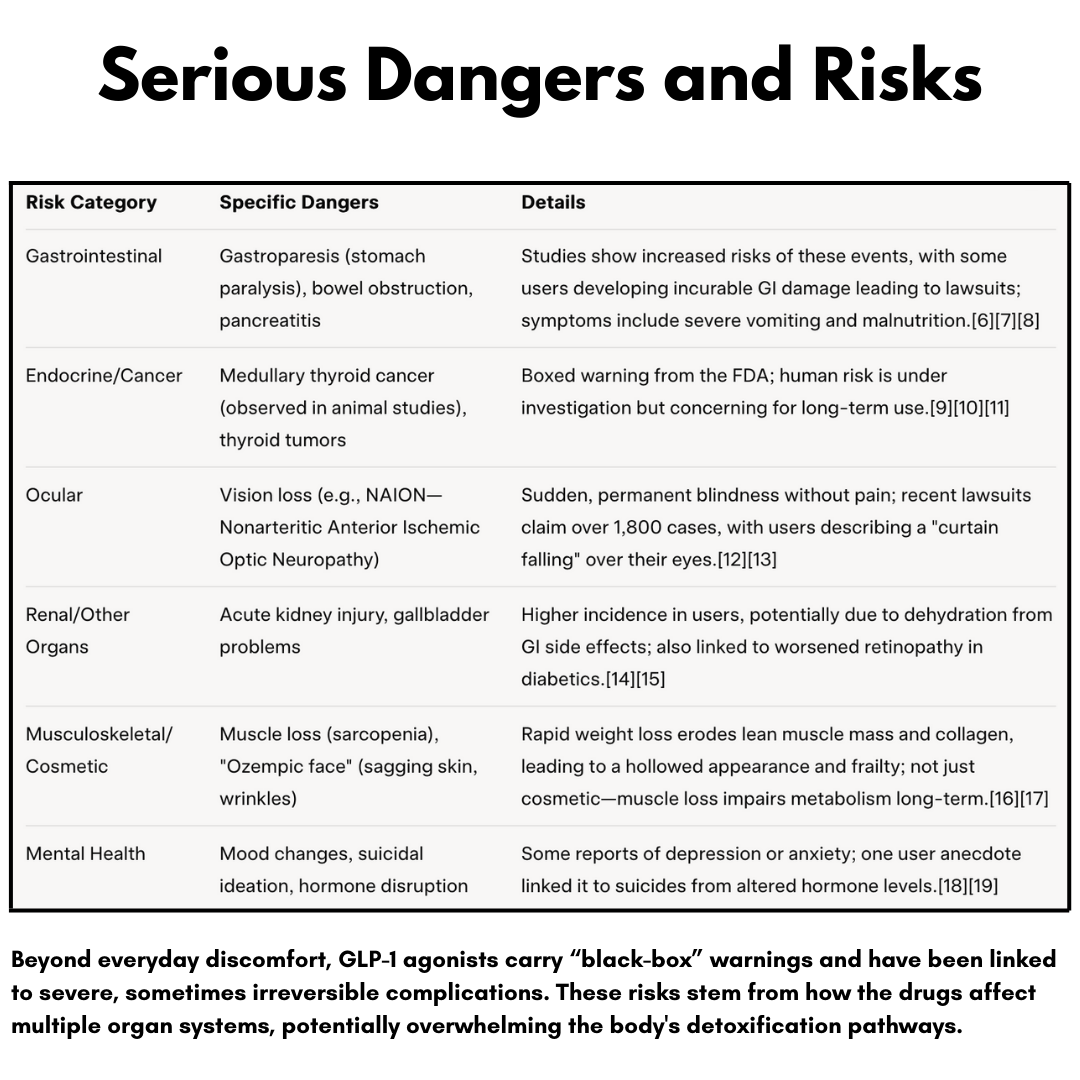
From how I see it, these dangers highlight how overriding the body’s signals (like appetite and digestion) can cascade into systemic imbalance. For instance, slowing gastric emptying might control blood sugar temporarily but stresses the pancreas and kidneys, potentially accelerating the diseases it’s meant to manage.
Other Reasons to Avoid GLP-1 Agonists
Even without side effects, these drugs aren’t aligned with holistic health principles:
- They Don’t Address Root Causes: Weight gain and diabetes often stem from insulin resistance driven by processed foods, stress, poor sleep, toxin exposure, or hormonal disruptions (e.g., thyroid or cortisol issues). GLP-1 drugs artificially suppress hunger without healing these, and patients often regain weight upon stopping, sometimes more than before.[26][27] I tend to focus on personalized protocols like anti-inflammatory diets (e.g., Mediterranean or low-carb), gut-healing probiotics, and stress reduction to restore natural GLP-1 production.
- Dependency and Rebound Effects: These are typically lifelong medications; discontinuation leads to rapid weight regain and potential metabolic worsening. This creates a cycle of reliance on Big Pharma, ignoring the body’s ability to self-regulate through lifestyle.
- High Cost and Access Issues: Often as much as $1,000+ monthly without insurance coverage for weight loss, leading to shortages that harm diabetics who need them most.[28] Ethical concerns arise from off-label use by celebrities, exacerbating inequities.[29]
- Potential for Misuse and Unknown Long-Term Impacts: With rising popularity, misuse (e.g., for non-medical weight loss) increases risks like nutrient deficiencies from reduced food intake. Emerging research suggests mixed effects on dementia (some decreased, others increased risks) and addiction, but long-term data are limited (since these drugs are relatively new).[30][31] User reports highlight horrors like permanent disability or death, underscoring that “miracle drugs” often come with hidden costs.[32][33]
- Mental Programming: Every time someone injects themself with this toxin, they are affirming in their own mind that they don’t have the willpower to control themselves, making an already present assumption worse. This is the opposite of the programming they should be doing in order to achieve a permanent solution on their own by changing their own habits and patterns. No one is overweight because of a deficiency in synthetic Gila monster venom. It is often due to their habits, patterns, cravings, and other brain functions that can be addressed and reversed.
- Gastrointestinal Paralysis: Ozempic has a half-life of seven days (compared to five minutes for natural GLP-1), which can permanently paralyze the digestive tract.
Weight Regain After Stopping GLP-1 Drugs: The Rebound Reality
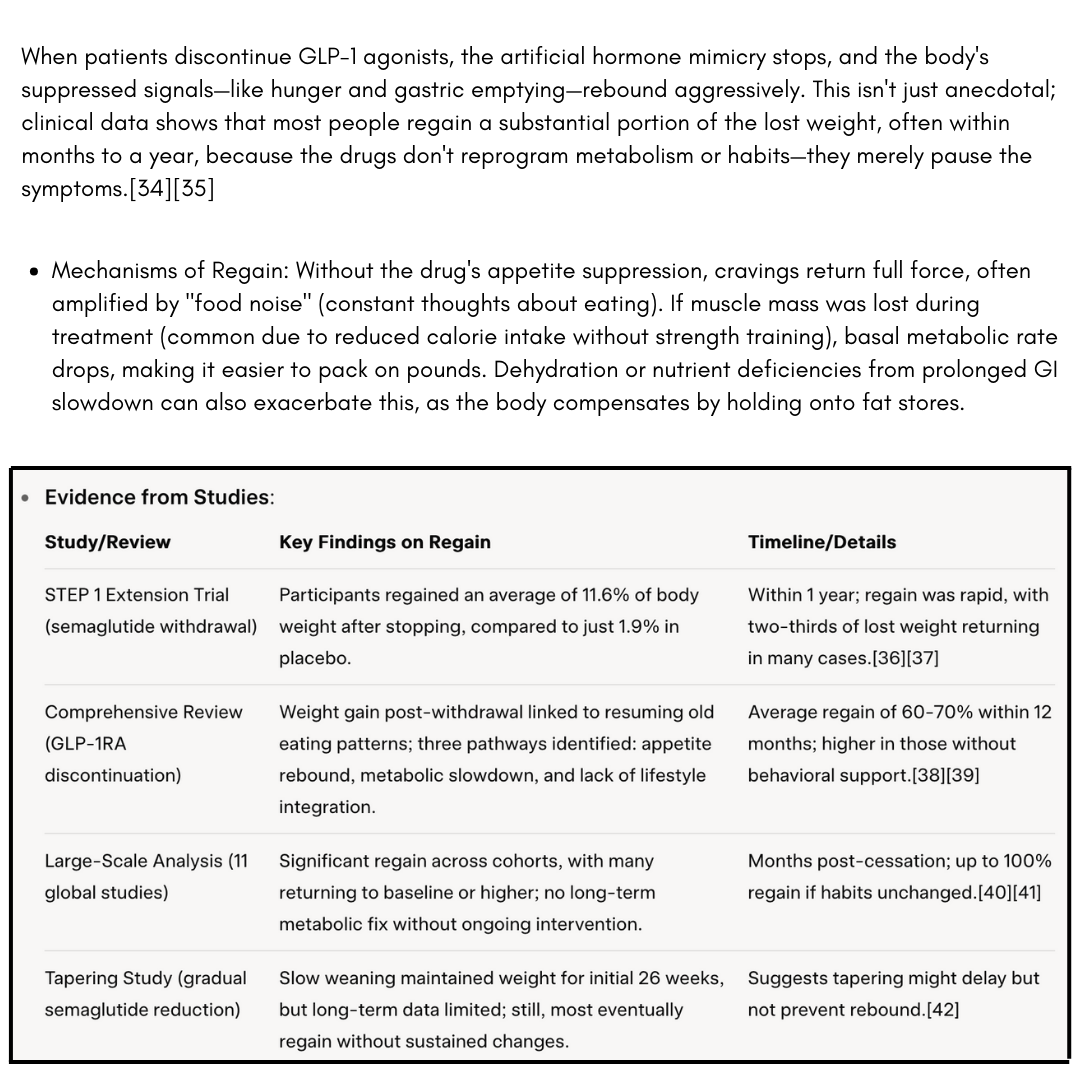
From user experiences shared online, this rebound weight gain is disheartening: one person noted that stopping Ozempic leads to pounds returning “fast” because it doesn’t fix obesity, just suppresses appetite, creating lifelong dependency.[43] Another highlighted that 95% of dieters (including drug users) regain weight within 5 years, calling it a “people problem” tied to unchanged habits.[44] Even bodybuilders using these drugs report bulking possible, but only with intentional protein focus and training—without that, regain is inevitable.[45] It would be easy for most to see this as a sign that the body is reverting to its setpoint, unaltered by the drug’s temporary override.
To mitigate regain, some evidence points to combining cessation with immediate lifestyle ramps: high-protein diets (1-2g/kg body weight), resistance training 2-3x/week (like X Gym), and cardio like walking or biking.[46][47] But honestly, if you’re already building those habits, why rely on the drug at all?
Using GLP-1 Drugs as a Shortcut: Bypassing True Behavior Change
These medications are frequently marketed as a “game-changer” for weight loss, but they often serve as a crutch, allowing users to avoid the deeper work of habit overhaul. In holistic terms, this is like putting a band-aid on a leaky roof—it might stop the drip temporarily, but the structure remains weak. Research and patient stories reveal that while the drugs reduce intake, they rarely inspire the root-level shifts needed for autonomy, leading to dependency and disappointment.[48][49]
- Why It’s a Shortcut: GLP-1 agonists quiet “food noise” by mimicking satiety signals, but they don’t educate on why overeating happens (e.g., addictive foods, processed foods spiking insulin, emotional eating from stress, or microbiome imbalances). Without addressing these, users miss the opportunity to rewire their relationship with food. A review emphasizes that sustainable weight loss requires lifestyle integration, yet many view the drugs as a standalone solution, detracting from behavioral and environmental origins.[50] Health coaching alongside GLP-1s can help, but it’s underutilized; one study notes behavior changes are “essential” for long-term success, yet few prioritize them.[51]
- Few People Change Habits: Some users snack less or dine out infrequently while on the drugs, but these shifts often revert upon stopping, as the motivation was pharmacological, not intrinsic.[52] In reality, only a fraction adopt lasting changes like strength training or nutrient-dense eating; most rely on the drug’s effects without reflection. User anecdotes echo this: “A lot of the people I know on Ozempic learn nothing and still eat the garbage,” leading to no real metabolic improvement.[53] Even positive reports admit that without overhauling diet (e.g., stimulating natural GLP-1 with beef, eggs, or fiber), the benefits fade.[54][55] These drugs are literally doing the opposite of teaching people how to eat healthy and change their habits, by being the “lazy” way out and encouraging them to think of pharmaceuticals as a “cheat” that allows them to continue with their cravings and bad nutrition habits. It’s teaching them that they need “external willpower” to make up for their intrinsic lack. Subconsciously, the message is that they’re not enough, so they need a drug to compensate for their lack of willpower.
- Food Addictions Can Deepen: Most people report that their food addictions have not changed on GLP-1 agonist drugs. They still eat the same “core cravings” they did before they started taking the drug, but just less, and don’t feel “as guilty” for these indulgences. They are still addicted because of what that food does to their brain. This is the main reason people have food addictions in the first place – to medicate their brain out of a particular mood or state they’re in. So when they go off the drug, they then return to original amounts of these “core cravings,” but in many cases, even more because their brain is in a worse state now, as they feel helpless about the weight regain and tend to be in a deeper funk than before as their guilt increases again with increased intake of these foods, starting the mood/state cycle back up, but stronger.
The Trap of Eating Less Volume but the Same Poor Foods
This is spot-on and a common pitfall I warn about: the drugs curb portion sizes by enhancing fullness, but if the food quality stays the same—think processed carbs, sugary snacks, or inflammatory oils—the underlying issues persist. You’re essentially starving your body of nutrients while feeding it the same toxins, which doesn’t heal insulin resistance or inflammation. Post-drug, when appetite returns, those unchanged preferences lead straight to regain, often with added frustration.[56]
- How It Plays Out: Users get excited about eating “less” (e.g., half a pizza instead of a whole), but the nutrient-poor choices don’t boost natural GLP-1 or support muscle/thyroid health. Some studies on food preferences show some shift toward healthier options, but it’s inconsistent; most stick to familiar comfort foods, missing the chance to retrain taste buds.[57] This leads to micronutrient gaps (e.g., low protein causing muscle loss) and rebound hunger that’s harder to manage without the drug.[58] As one expert notes, GLP-1s make calorie deficits easier but don’t inherently promote better habits—users must intentionally choose high-fiber, protein-rich foods to sustain changes.[59]
- Similar to Type II Diabetics: For the overwhelming majority, taking insulin doesn’t cause Type II diabetics to start eating healthier. They discontinue with the foods they’re addicted to, using insulin as a crutch to continue. Even their doctors rarely give them advice on changing their nutritional habits. I have a friend who cares for type 2 diabetics with amputated limbs because of the extreme nature of their diabetes in their eating habits. She tries to counsel them, is unhealthy, and even points out they will lose the other foot if they don’t change what they eat, but the vast majority just say, “I know that will happen, but I just can’t do it.”
Better Natural Alternatives Exist
Instead of these drugs that have no effect on habits and lifestyle changes, consider evidence-based natural strategies:
- Dietary Shifts: High-fiber, low-glycemic foods (e.g., berries, leafy greens) naturally boost GLP-1.[60][61]
- Supplements: Berberine, cinnamon, or alpha-lipoic acid for blood sugar support; probiotics for gut health.[62]
- Lifestyle: Intermittent fasting, strength training, and stress management (e.g., meditation) to enhance insulin sensitivity without drugs.[63]
- Herbs: Bitter melon or fenugreek for metabolic balance.[64]
- The Brain Type Test: the reason I invented my brain type test was to help people with cravings, food, addictions, emotional leading, overeating, exercise, motivation, and more. Just click here to explore that option.
If you’re considering or currently on these drugs, consult a functional medicine provider to taper safely and transition to root-cause solutions. Your body has the blueprint for health—let’s unlock it naturally!
The bottom line is that food is highly addictive (especially processed food). In some studies, it’s even more addictive than cocaine.[65] [66] [67] [68] GLP-1 agonists don’t help with this. They only temporarily allow a person to eat less. Eating disorders – especially overeating and emotional eating are also rooted in addiction, and GLP-1 agonists can’t help with those either, for the same reason, and often make it worse later. This is also why people gain the weight back, the vast majority of the time, when they go off these drugs. See footnotes below [69-70] for more studies on this topic of addiction.
If a doctor prescribes GLP-1 agonists, they should only prescribe them in extreme and rare cases, and only under the condition that a qualified behavior modification therapist counsels the patient. If behavior modification is successful and addictions are broken, the patient will not need to be on these drugs for extended periods of time and will have success in keeping the weight off after discontinuing the drugs.
Lastly, if your doctor is willing to prescribe these drugs to you without full informed consent of the benefits (one) and risks (many known and certainly more unknown), including making sure that you thoroughly read the package insert from the drug manufacturer, run, screaming from that doctor! They do not have your best interests in mind, and they are violating their oath to “Do no harm.” Remember, this is a new drug that has not been properly tested, with the longest (observational) study being only 5 years.[71] The only people I might recommend this class of drugs to (for 6 months, max) are those who already have their bariatric surgery appointment scheduled, who are committed to that option, and there’s no other way to talk them out of it. Then I would work with them while they are on it, with intensive brain training, to help them get past the addictions and eating disorders that caused them to get to where they are.
These drugs are still relatively new, not adequately tested, and have only been used off-label for weight loss on a large scale since 2020, with it turning into a fad around 2021. Mark may words: THIS WILL NOT END WELL! There are already massive lawsuits being filed, and there will be more. Many practitioners who prescribe them will also be sued (at worst) or just look really stupid (at best). If this post has talked you out of taking these drugs, you will thank me in the future – guaranteed!
P.S. The Gila Monster Venom Connection: Inspiration, Not Ingredient
Some sensationalist internet “influencers” claim there is Gila monster venom in these drugs. The discovery of these drugs traces back to research on Gila monster venom in the 1980s and 1990s. Scientists, including Dr. John Eng and Dr. Jean-Pierre Raufman, found that the venom contains a peptide called exendin-4, which shares structural and functional similarities with human GLP-1 but is far more stable, lasting hours in the body compared to GLP-1’s mere minutes. This stability made exendin-4 an ideal candidate for drug development.
- How It Started: In the 1980s, researchers like Dr. Paul Raufman tested Gila monster venom on guinea pig pancreases and noticed it triggered strong insulin release, mimicking GLP-1’s effects. By the 1990s, Dr. Eng isolated exendin-4, and Dr. Daniel Drucker’s team at the University of Toronto confirmed its potential by studying a Gila monster from the Utah Zoo. This led to the development of exenatide (Byetta), the first GLP-1 agonist, approved by the FDA in 2005 for type 2 diabetes. Semaglutide, used in Ozempic and Wegovy, was a later advancement, building on this research to create a longer-acting synthetic molecule.
- Clarification: No Gila monster venom is used in the actual manufacturing of these drugs. Instead, pharmaceutical companies create synthetic versions of exendin-4 or related peptides. The venom served as a blueprint, not an ingredient. Claims on platforms like X suggesting that Ozempic is “Gila monster venom” are misleading exaggerations, though they stem from this scientific history. For example, one X post inaccurately called semaglutide “the active ingredient in Gila monster venom,” while another clarified it’s inspired by exendin-4 in the lizard’s saliva, not venom itself.
From a functional health perspective, this origin story raises red flags. While nature often provides healing compounds (e.g., plant-based remedies like willow bark for aspirin), repurposing a toxin from a venomous lizard into a synthetic drug that overrides the body’s natural systems feels like a departure from holistic principles. The Gila monster’s venom evolved to immobilize prey, not to slow human digestion. Mimicking its effects might yield results, but it ignores the body’s innate ability to regulate GLP-1 through diet, exercise, and stress management—approaches that don’t carry the same risks or dependency.
Footnotes
[1] GLP-1 diabetes and weight-loss drug side effects – Harvard Health – https://www.health.harvard.edu/staying-healthy/glp-1-diabetes-and-weight-loss-drug-side-effects-ozempic-face-and-more
[2] 19 Semaglutide (Ozempic, Wegovy) Side Effects You … – GoodRx – https://www.goodrx.com/ozempic/semaglutide-side-effects?srsltid=AfmBOoozu42gPwjODVqryB-_GI8P_XIoyVGy7fJW6zEMbBU0eDn4JSAL
[3] Possible Side Effects of Ozempic ® (semaglutide) Injection – https://www.ozempic.com/how-to-take/side-effects.html
[4] 10 GLP-1 Side Effects You Should Know About – GoodRx – https://www.goodrx.com/classes/glp-1-agonists/glp-1-side-effects?srsltid=AfmBOoqiWcaAEkPrbZ-saoEAtqbctExrcheelvLGSjWOnzJMqsErvEzH
[5] Semaglutide: Uses, Dosage, Side Effects, Brands – Drugs.com – https://www.drugs.com/semaglutide.html
[6] GLP-1 Agonists and Gastrointestinal Adverse Events – JAMA Network – https://jamanetwork.com/journals/jama/fullarticle/2810542
[7] 10 GLP-1 Side Effects You Should Know About – GoodRx – https://www.goodrx.com/classes/glp-1-agonists/glp-1-side-effects?srsltid=AfmBOorXuSbyE4gJ3lSk5NHcV0slAYbz3FO9kuaW9fyaWqoNl2JV6f0J
[8] Researchers link popular weight loss drugs to serious digestive … – https://www.cnn.com/2023/10/05/health/weight-loss-drugs-serious-digestive-problems-study
[9] Do GLP-1–Based Therapies Increase Cancer Risk? – PMC – https://pmc.ncbi.nlm.nih.gov/articles/PMC3920789/
[10] Semaglutide Injection: MedlinePlus Drug Information – https://medlineplus.gov/druginfo/meds/a618008.html
[11] Is Semaglutide Linked to Cancer? What Studies Say | Atraxia Law – https://www.atraxialaw.com/news/is-semaglutide-linked-to-cancer-what-studies-say/
[12] Semaglutide or Tirzepatide and Optic Nerve and Visual Pathway … – https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2837377
[13] Ozempic Lawsuit | August 2025 Latest Litigation Update – https://www.lawsuit-information-center.com/ozempic-gastroparesis-lawsuit.html
[14] Tirzepatide Deaths | Fatal Side Effects of GLP-1 RA Medications – https://www.motleyrice.com/diabetes-lawsuits/tirzepatide/deaths
[15] Trulicity Lawsuit – August 2025 Update | King Law – https://www.robertkinglawfirm.com/personal-injury/trulicity-lawsuit/
[16] Ozempic face (and other GLP-1 side effects) – UCLA Health – https://www.uclahealth.org/news/article/ozempic-face-and-other-glp-1-side-effects
[17] GLP-1 Agonists – Cleveland Clinic – https://my.clevelandclinic.org/health/treatments/13901-glp-1-agonists
[18] Semaglutide: Double-edged Sword with Risks and Benefits – PMC – https://pmc.ncbi.nlm.nih.gov/articles/PMC11790292/
[19] A new era of weight loss: Mental health effects of GLP-1 drugs – https://www.apa.org/monitor/2025/07-08/weight-loss-drugs-mental-health
[20] Ozempic Lawsuit (August Update) | Oberheiden P.C. – https://federal-lawyer.com/injury-lawsuit/ozempic/
[21] Ozempic Lawsuit | August 2025 Latest Litigation Update – https://www.lawsuit-information-center.com/ozempic-gastroparesis-lawsuit.html
[22] FDA’s Concerns with Unapproved GLP-1 Drugs Used for Weight Loss – https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/fdas-concerns-unapproved-glp-1-drugs-used-weight-loss
[23] Ozempic Lawsuits – mctlaw – https://www.mctlaw.com/product-liability/glp-1/ozempic-lawsuits-semaglutide/?srsltid=AfmBOorptHyAlYmiGIug5wULOmc86S8EWWu1kDR_hi5J_u3jfa1pwWva
[24] Weight loss injections and cancer: 6 questions, answered – https://www.mdanderson.org/cancerwise/weight-loss-injections-and-cancer–6-questions–answered.h00-159702279.html
[25] Who Shouldn’t Take GLP-1 Medications? – GoodRx – https://www.goodrx.com/classes/glp-1-agonists/who-should-not-take-glp-1?srsltid=AfmBOor5JFXU1fglUoR8ngdgyJNZSNZmKWZNKV3NuPPgawhQInPPF9Lx
[26] Weight regain and cardiometabolic effects after withdrawal of … – https://pubmed.ncbi.nlm.nih.gov/35441470/
[27] The Data Are Clear: Patients Regain Weight After Stopping GLP-1 … – https://www.medpagetoday.com/special-reports/exclusives/112138
[28] The new obesity drugs work, but it’s a dilemma when people have to … – https://www.npr.org/2024/05/27/nx-s1-4930028/ozempic-wegovy-zepbound-mounjaro-glp1-obesity-weight-loss-regain
[29] Ozempic® Lawsuit | August 2025 Latest Legal Updates – Motley Rice – https://www.motleyrice.com/diabetes-lawsuits/ozempic
[30] Emergency Presentations of GLP-1 Agonist Complications – https://www.nuemblog.com/blog/glp1-complications-goins
[31] Do New Obesity and Diabetes Drugs Also Curb Drinking, Gambling … – https://www.bu.edu/articles/2025/diabetes-drugs-also-curb-addictions/
[32] Tirzepatide Deaths | Fatal Side Effects of GLP-1 RA Medications – https://www.motleyrice.com/diabetes-lawsuits/tirzepatide/deaths
[33] Ozempic Lawsuit – August 2025 Update – King Law – https://www.robertkinglawfirm.com/personal-injury/ozempic-lawsuit/
[34] Does Stopping Ozempic Cause Rebound Weight Gain and Health … – https://www.scientificamerican.com/article/does-stopping-ozempic-cause-rebound-weight-gain-and-health-problems/
[35] Many Patients Maintain Weight Loss a Year After Stopping … – https://epicresearch.org/articles/many-patients-maintain-weight-loss-a-year-after-stopping-semaglutide-and-liraglutide
[36] Weight regain and cardiometabolic effects after withdrawal of … – https://pubmed.ncbi.nlm.nih.gov/35441470/
[37] Weight regain and cardiometabolic effects after withdrawal of … – https://dom-pubs.onlinelibrary.wiley.com/doi/10.1111/dom.14725
[38] Trajectory of the body weight after drug discontinuation in the … – https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-025-04200-0
[39] The Data Are Clear: Patients Regain Weight After Stopping GLP-1 … – https://www.medpagetoday.com/special-reports/exclusives/112138
[40] People who stop weight loss drugs return to original … – The Guardian – https://www.theguardian.com/society/2025/may/14/people-who-stop-weight-loss-drugs-return-to-original-weight-within-year-analysis-finds
[41] Discontinuing glucagon‐like peptide‐1 receptor agonists and body … – https://onlinelibrary.wiley.com/doi/10.1111/obr.13929
[42] Is coming off semaglutide slowly the key to preventing weight regain? – https://easo.org/is-coming-off-semaglutide-slowly-the-key-to-preventing-weight-regain/
[43] Avoiding weight regain after GLP-1 medication – YouTube – https://www.youtube.com/watch?v=pUWAgJKkOlg
[44] Discontinuation and Reinitiation of GLP-1 Receptor Agonists – https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2829779
[45] Weight Regain After Liraglutide, Semaglutide or Tirzepatide … – MDPI – https://www.mdpi.com/2077-0383/14/11/3791
[46] How to Keep the Weight Off After Stopping Semaglutide – Healthline – https://www.healthline.com/health/how-to-keep-weight-off-after-semaglutide
[47] Coming off GLP-1s slowly could be key to preventing weight regain – https://www.pharmacist.com/APhA-Press-Releases/coming-off-glp-1s-slowly-could-be-key-to-preventing-weight-regain
[48] Semaglutide and Empty Promises of Change – Psychology Today – https://www.psychologytoday.com/us/blog/understanding-health-behaviors/202409/semaglutide-and-empty-promises-of-change
[49] GLP-1s vs. Behavior Change: What Drives Lasting Weight Loss – https://www.fitonhealth.com/blog/glp-1s-vs.-behavior-change-what-drives-lasting-weight-loss
[50] GLP-1s or Behavior Change? Unlocking The Winning Formula for … – https://www.welldoc.com/glp-1s-or-behavior-change-unlocking-the-winning-formula-for-sustainable-weight-loss/
[51] Health and Well-Being Coaching Adjuvant to GLP-1 Induced Weight … – https://pmc.ncbi.nlm.nih.gov/articles/PMC11577329/
[52] GLP-1 Use Reveals Lasting and Positive Behavioral Changes – https://www.pbahealth.com/elements/glp-1-use-reveals-lasting-behavioral-changes/
[53] Moving Forward Without GLP-1: A Behavioral Approach to Lasting … – https://www.pritikin.com/your-health/moving-forward-without-glp-1-a-behavioral-approach-to-lasting-health.html
[54] How Biosensor-Driven Apps Are Shaping the GLP-1 Ecosystem – https://sequenex.com/biosensor-driven-apps-and-glp-1-ecosystem/
[55] GLP-1 Use Reveals Lasting and Positive Behavioral Changes – https://www.pbahealth.com/elements/glp-1-use-reveals-lasting-behavioral-changes/
[56] Semaglutide and Empty Promises of Change – Psychology Today – https://www.psychologytoday.com/us/blog/understanding-health-behaviors/202409/semaglutide-and-empty-promises-of-change
[57] GLP-1s vs. Behavior Change: What Drives Lasting Weight Loss – https://www.fitonhealth.com/blog/glp-1s-vs.-behavior-change-what-drives-lasting-weight-loss
[58] The new obesity drugs work, but it’s a dilemma when people have to … – https://www.npr.org/2024/05/27/nx-s1-4930028/ozempic-wegovy-zepbound-mounjaro-glp1-obesity-weight-loss-regain
[59] GLP-1s or Behavior Change? Unlocking The Winning Formula for … – https://www.welldoc.com/glp-1s-or-behavior-change-unlocking-the-winning-formula-for-sustainable-weight-loss/
[60] 9 Foods and Supplements That Increase GLP-1 Naturally – GoodRx – https://www.goodrx.com/conditions/weight-loss/how-to-increase-glp-1-naturally?srsltid=AfmBOopQ8VceVa7CNPHLQuCw9KsXG2zD55_bcelGuRbgM4N6FjOz11mm
[61] Can You Boost GLP-1 Naturally? – WebMD – https://www.webmd.com/obesity/features/natural-glp1-boosters
[62] GLP-1 Alternatives | Root Functional Medicine – https://rootfunctionalmedicine.com/glp1-alternatives
[63] 8 Natural Alternatives to Ozempic for Weight Loss | Take Care by Hers – https://www.forhers.com/blog/natural-alternatives-to-ozempic
[64] “Nature’s Ozempic”: The truth about natural GLP-1 supplements – https://wellworthy.com/natures-ozempic-natural-glp-1-supplements/
[65] Volkow, N. D., et al. (2001). “Brain dopamine and obesity.” The Lancet. – https://pubmed.ncbi.nlm.nih.gov/11210998/
[66] Wang, G. J., et al. (2002). “Brain dopamine and reward.” Annual Review of Neuroscience. – https://pubmed.ncbi.nlm.nih.gov/12052914/
[67] Stice, E., et al. (2010). “Relation between obesity and blunted striatal response to food.” Journal of Abnormal Psychology – https://pubmed.ncbi.nlm.nih.gov/20853907/
[68] Gearhardt, A. N., et al. (2011). “Neural correlates of food addiction.” Archives of General Psychiatry – https://pubmed.ncbi.nlm.nih.gov/21464344/
[69] Volkow, N. D., et al. (2013). “The addictive dimensionality of obesity.” Biological Psychiatry – https://pubmed.ncbi.nlm.nih.gov/23374642/
[70] Schulte, E. M., et al. (2016). “Which foods may be addictive? The roles of processing, fat content, and glycemic load.” – PLoS ONE. https://pubmed.ncbi.nlm.nih.gov/25692302/
[71] Marso, S. P., et al. (2016). “Liraglutide and Cardiovascular Outcomes in Type 2 Diabetes.” New England Journal of Medicine. https://www.nejm.org/doi/full/10.1056/NEJMoa1603827
For a great DEEP dive, see this article: https://eccentrik.substack.com/p/something-strange-is-happening-to